Discover HKBU
Can non-alcoholic fatty liver disease be cured? HKBU research offers hope
8 Nov 2023
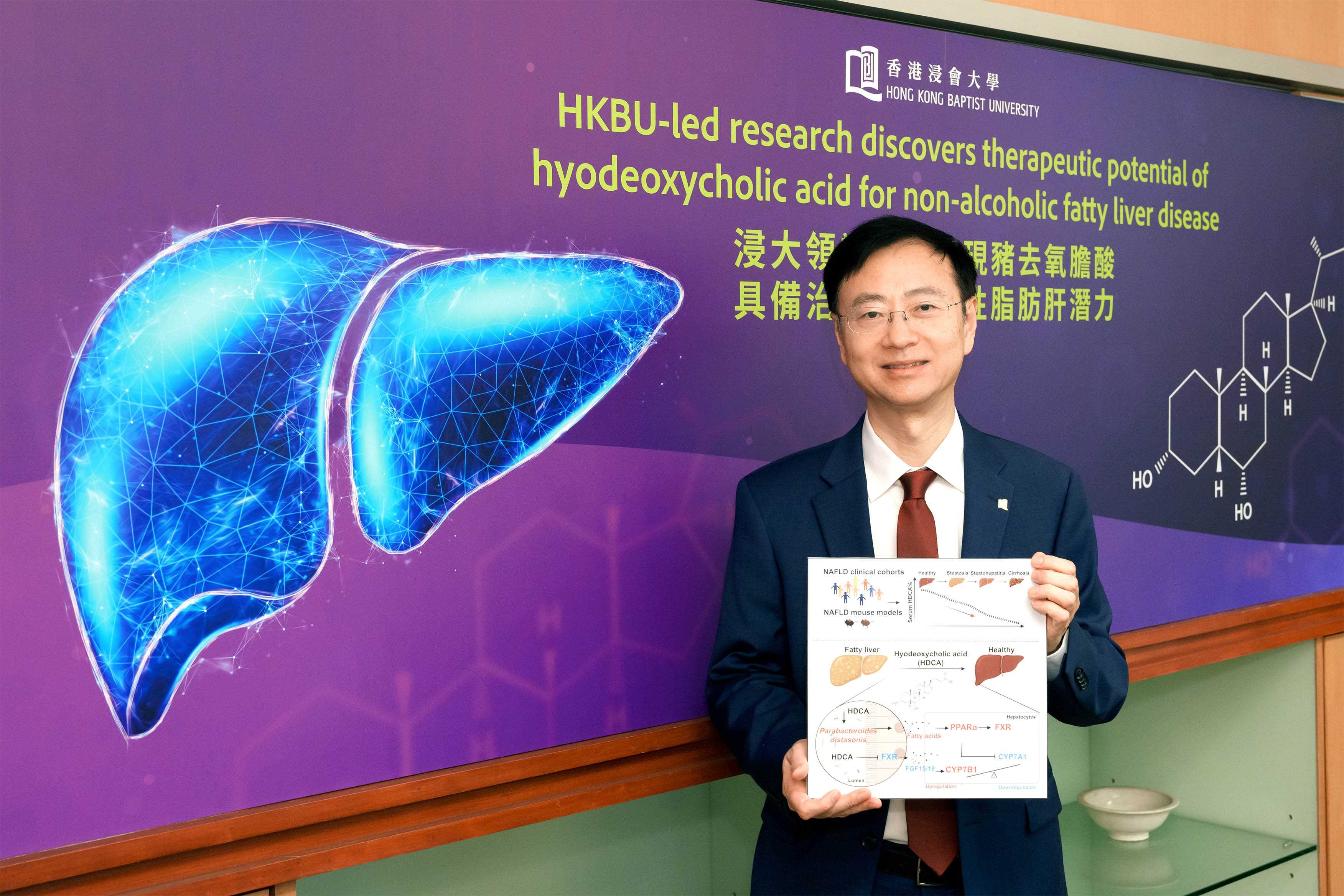
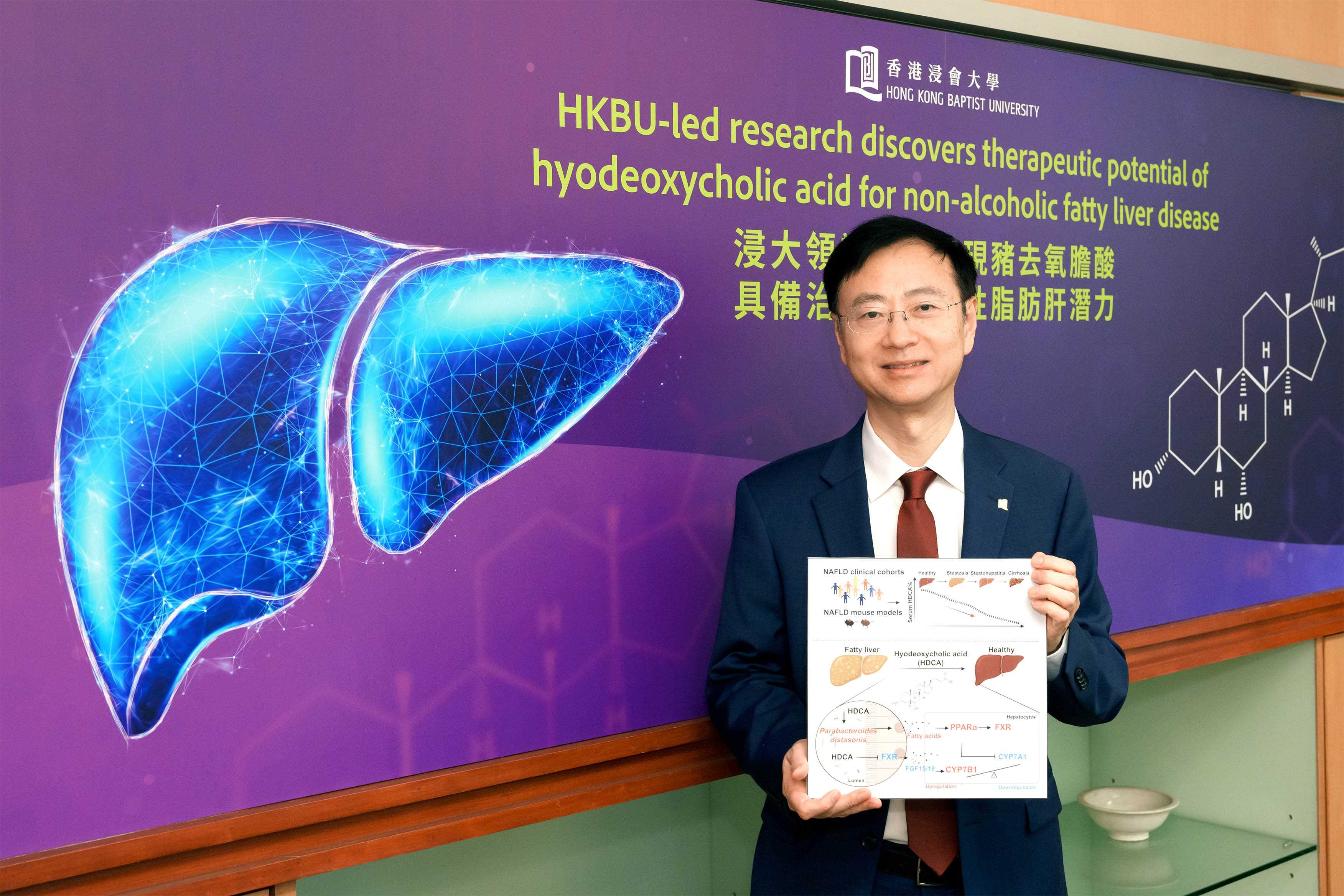
Non-alcoholic fatty liver disease (NAFLD) is a leading cause of chronic liver disease, affecting 32% of the adult population worldwide, yet there are no therapeutic drugs available for sale on the market for non-alcoholic steatohepatitis. New research led by HKBU offers hope of a potential therapeutic intervention.
The research team discovered that hyodeoxycholic acid (HDCA), a bile acid generated in human intestine, can reduce fat accumulation and inflammation in the liver. The findings, published in the renowned scientific journal Cell Metabolism, showed that HDCA’s intervention in NAFLD works by reshaping the population of beneficial gut bacteria, which affects the metabolic interactions between the gut and the liver.
“Our research is a significant stride forward in understanding the pathophysiology of NAFLD, and it offers a potential new avenue for therapeutic intervention,” says Professor Jia Wei, Acting Dean and Chair Professor in Chinese Medicine and Systems Biology of the School of Chinese Medicine at HKBU, who led the study.
The researchers found that individuals with NAFLD have lower levels of HDCA compared to those without NAFLD. A series of controlled experiments were then conducted to evaluate HDCA’s therapeutic potential.
The team orally fed HDCA to mouse models with NAFLD for eight weeks. The results showed that HDCA markedly reduced excessive lipid droplets, and improved hepatic inflammation, oral glucose tolerance, and insulin sensitivity compared to the control group. It was also found that HDCA alleviated NAFLD conditions and the risk factors of NAFLD such as type 2 diabetes and insulin resistance.
Interestingly, HDCA did not exert its therapeutic effects on NAFLD by directly targeting liver cells. The researchers hypothesised that HDCA induced gut microbiota alterations, which might contribute to the alleviation of NAFLD. Further studies revealed that HDCA provided a favourable environment for the thriving of Parabacteroides distasonis, a member of the core microbiome in the human gut, which regulates fatty acid metabolism as well as the hepatic bile acid synthesis pathways.
Looking ahead, HKBU researchers will coordinate a phase I and II clinical trial in the Mainland to evaluate the safety and efficacy of HDCA for patients with fatty liver disease and type 2 diabetes.
“The study underscores the crucial role of the gut-liver metabolic axis in disease management. We hope that the research findings on HDCA and the clinical trial to be conducted in the Mainland will provide more insights into the treatment of fatty liver disease and non-alcoholic steatohepatitis,” says Professor Jia.