Discover HKBU
New discovery unveils therapeutic target for COVID-19
28 Mar 2023
In the past few years, the development of COVID-19 vaccines and drugs topped the task list of the scientists as a result of the global outbreak of this pandemic. Two major challenges when it comes to developing COVID-19 drugs are how to enhance treatment results for patients with weak immune systems, and how to maintain the drugs’ effectiveness across different viral strains. Understanding the cell entry mechanism of SARS-CoV-2 virus is vital to curb the spread of the virus, and it will also aid the search for new COVID-19 treatments.
SARS-CoV-2 requires angiotensin-converting enzyme 2 (ACE2), a protein found on the membrane of human cells, as its receptor for cellular entry. Previous studies found that the infection of organs with low levels of ACE2 expression by SARS-CoV-2 is made possible by a soluble form of ACE2. The soluble ACE2 binds with SARS-CoV-2, carries the virus to cells with low levels of ACE2 expression, and facilitates its entry into the cells.
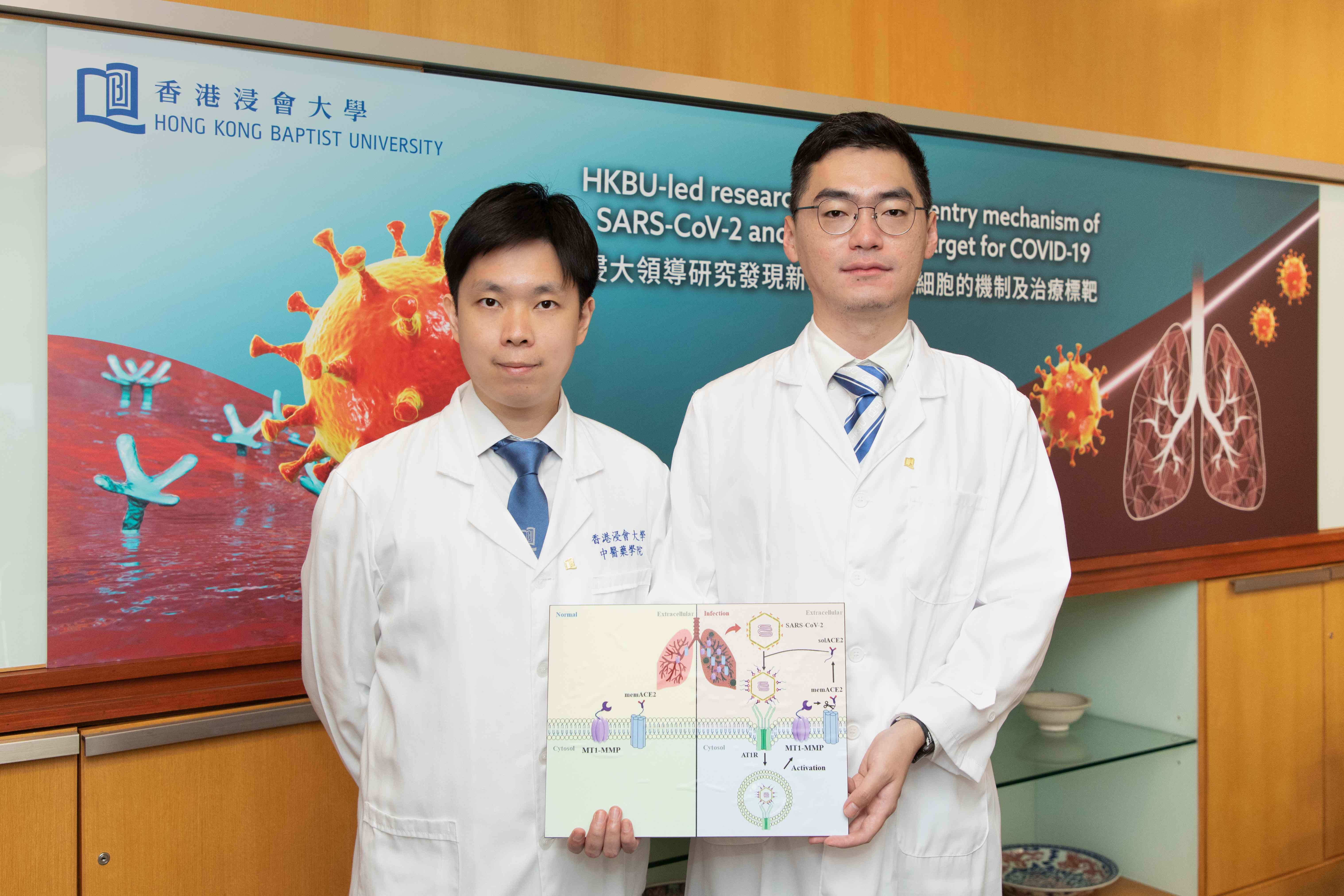
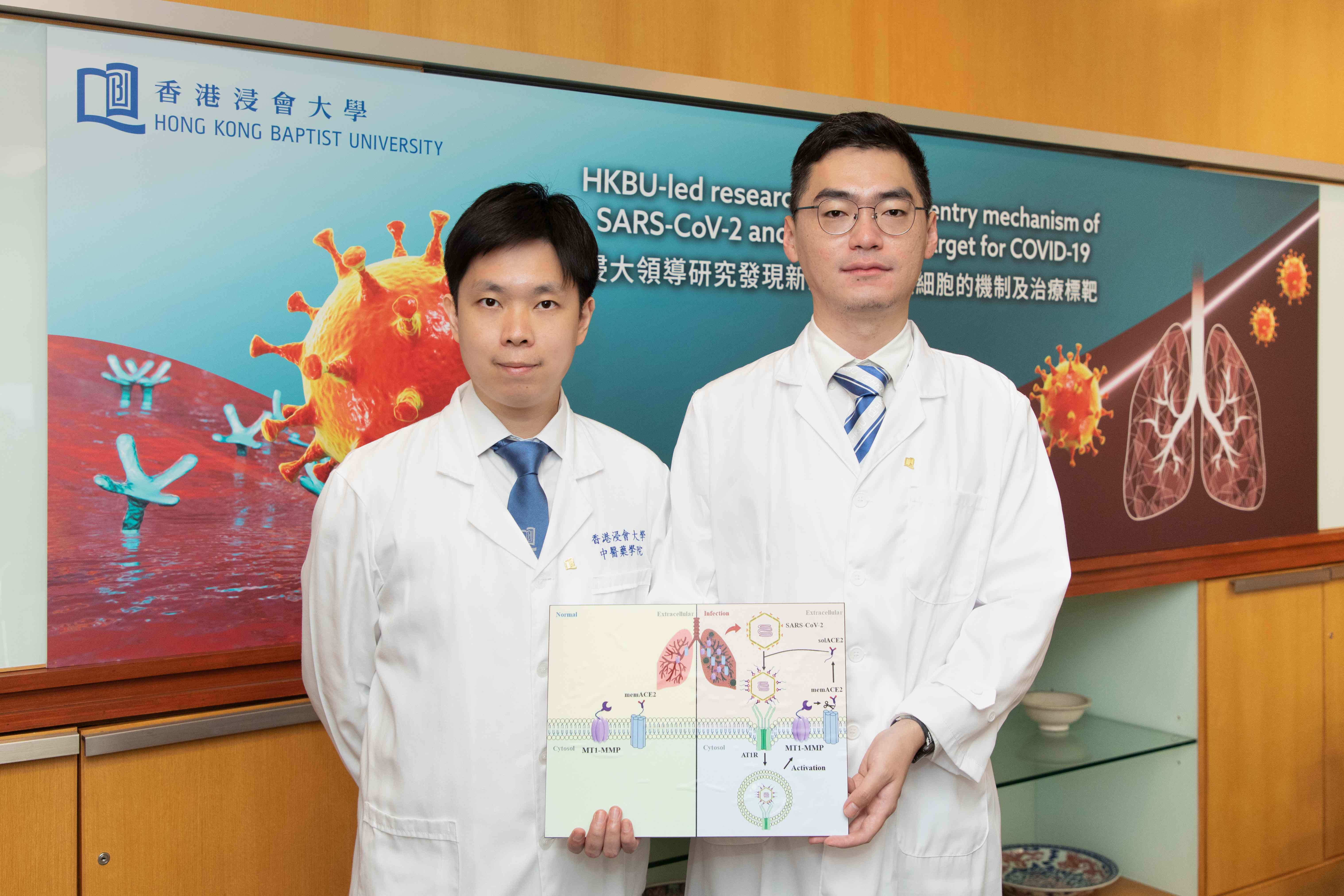
A research team led by Dr Xavier Wong, Assistant Professor of the School of Chinese Medicine at HKBU, in collaboration with Dr Yuan Shuofeng, Assistant Professor of the Department of Microbiology at The University of Hong Kong, studied how the physiological regulation of soluble ACE2 shedding contributes to the aetiology of COVID-19.
MT1-MMP mediates cell entry of SARS-CoV-2
The team found that SARS-CoV-2 infection leads to the increased activation of MT1-MMP, a protease crucial for many physiological processes. MT1-MMP mediates the release of soluble ACE2 from ACE2-expressing cells, and the soluble ACE2 in turn binds to the spike proteins of SARS-CoV-2 and carries it to the uninfected cells with low levels of ACE2 expression.
Notably, the team demonstrated that the introduction of human-soluble ACE2 enables SARS-CoV-2 to infect the lungs of a laboratory mouse strain (C57BL/6 mice) that is naturally insusceptible to SARS-CoV-2 infection due to the incompatibility of its mouse ACE2 and the viral spike proteins. The findings unveil the mechanism by which the virus hijacks host enzymes to enhance its infectivity, triggering multi-organ infections.
Antibody 3A2 blocks MT1-MMP activity
To study MT1-MMP’s functions and how it affects viral infection, the researchers used human cells to create organoids, a 3D tissue structure grown in vitro to resemble and model different organs in the laboratory.
They discovered that blocking MT1-MMP activity with the monoclonal antibody 3A2 effectively depletes soluble ACE2 levels and reduces the degree of infection of SARS-CoV-2 in human lung, heart and liver organoids by 60-80%. Consistent results were obtained using the original strain of SARS-CoV-2, as well as variants of concern, such as Delta and Omicron. The results demonstrate that MT1-MMP is a major host factor that mediates the cell entry of SARS-CoV-2, and also a potential therapeutic target for COVID-19 drugs. The research findings have been published in Nature Communications.
The researchers further tested the effects of applying 3A2 in a mouse COVID-19 model. Older mice were used in the experiment as old age is a major risk factor for severe symptoms and mortality for COVID-19. The results show that 3A2 reduced the viral load of SARS-CoV-2 by almost 90% and dramatically alleviated lung tissue damage resulting from infection.
MT1-MMP as a therapeutic target
Dr Wong says: “3A2 has good potential to become an effective drug for curing COVID-19 because it antagonises the activity of MT1-MMP, instead of boosting the immunity of patients or acting directly on the virus.
“Our previous studies have demonstrated that 3A2 also offers protection against obesity and diabetes, two major risk factors for severe symptoms and mortality for COVID-19. Therefore, 3A2 could be particularly suitable for high-risk groups, including older adults and people with metabolic disorders. It could also be effective against emerging coronaviruses in the future, because ACE2 is a doorway for many such viruses with similar cell entry mechanisms. Further research and experiments on 3A2 are required before it can be applied in humans.”